Show notes + Transcript
Emily: I’m Emily Kumler and this is Empowered Health. This week on Empowered Health, we’re going to be talking about diabetes. This is a really important topic because they don’t think that most people realize that 50% of Americans right now have diabetes or have pre-diabetes. This is costing the country more than $300 billion dollars. That’s billion with a B in care. And it’s possible that people don’t even need medicine for this. Everybody’s been diagnosed with these diseases gets put on insulin, and there’s a company called Virta Health that’s been looking at this problem and figuring out that maybe by changing things in your diet, you can control your blood sugar enough that you don’t need any outside insulin or other medications. Okay, so we’re gonna start off by talking to one of the first patients in the Virta trial. Here is Kim Shepherd. She’s 58. Do you remember how much money you were spending on medications?
Kim: It was about $158 a month. I’m off of 10 prescription medications in this three year study and that doesn’t even count the Toujeo because I was not paying for that. I was still in the using the doctor sample pins, but I did call my pharmacy to see how much it would be. And it was $258 a pen. And where I had gotten to in that point, I was on two pens a month. So we’re talking about almost tripling my prescription costs. Had I had to stay on the Toujeo.
Emily: So you saw an ad in the newspaper for the Virta study and do you remember what it said?
Kim: It’s a diabetes study, I had been on that Tuesday open about a month, maybe, maybe six weeks. It was miserable. I mean you’re sticking your stomach, you’re injecting the pen right into your stomach. So then you lean against something, you’re stomach is tender. It was just miserable. And I just thought, I can’t do this. And my uncle’s a diabetic and he’s always an insulin taking diabetic. And I would see him at family parties having to measure how much insulin he needs and just, I was projecting myself into that future and I just thought I can’t do this. I saw the study and it was, and it was, you know, they were doing 200 remote, I’m in Indianapolis, so I was in the remote and it was in Lafayette. And so I went up to Lafayette, it’s an hour, 30 minute drive from Indy to just talk to Dr. Hallberg see what this was about. And she gave me encouragement. Honestly, it’s the first health encouragement I’ve probably had in 10 years and I was 328 pounds and still had a 268 fasting blood sugar. But I honestly, I mean her enthusiasm for the project gave me hope and how that worked in the study. So you get your stuff and we have a scale and it goes up into the cloud. It’s magic. You don’t even have to look at the scale if you don’t want. They said when you onboard into the program and did the food part and that’s all it is, is food. She took me immediately that very first off of the Toujeo. Oh, I stopped taking it and I asked her, I’m like, my doctor at homes that I’m no longer producing insulin, so how’s this going to work? And she’s like, trust me. I’m like, okay. She gave me hope.
Emily: That’s a lot of trust, right? Like that sort of sounds terrifying in a way.
Kim: It was, it was an, I’m an hour or 20 minutes away from her office. So you know, like okay I’m going to go with this. They’d had some people that had already been in the studies, so that was in the newspaper. You know, one guy had gone off his meds and he was doing great and at this point I’m willing to grasp at anything to get better health. And my whole outlook for being in this study has, the health part comes first and the weight loss is second. I went off the Toujeo immediately and in that first week my blood sugar was dropping a hundred points from breakfast to lunch and she took me cause she’d cut the glipizide and half and then that first week she took me off of Glipizide completely, so I’d been on Glipizide probably almost 10 to 12 years and in the first week of just the diet controlled carb, low carb, I was off two medications being right there. That was amazing. I was like, what? And I felt fine.
Emily: I thought it was important for us to have a medical definition of what diabetes is. I’ve heard that it’s an intolerance to carbohydrates, but I was curious to hear from the medical director of the Joslin Diabetes Center as to how he would define it. Here is Dr. Gabbay.
Dr. Gabbay: There are two main types and type two is by far the most common. 90% of people have type two diabetes and type two develops because of two issues. The first issue is becoming resistant to the effects of insulin. And that happens from being overweight from a sedentary lifestyle and there’s a genetic component to that. So a family history, diabetes makes you more likely to have resistance to insulin. And insulin is a hormone that helps control people’s blood sugar. So first problem is becoming resistant to insulin and about a quarter of the U.S. population is in that space. Most of them make extra insulin to compensate for that resistance. And their blood sugars are normal and they don’t have diabetes, but they are at increased risk for heart disease and cardiovascular. What determines who develops diabetes is that first problem of insulin resistance. And then a second problem is the inability to continue to make the extra needed. And so they have a problem with their ability to make it, in addition to be resistant to it and as a result, their blood sugars rise and then they’re diagnosed with diabetes. And the medicines we use largely work many of them either by helping the body make for insulin or be less resistant.
Emily: Dr. Sarah Hallberg is the chair of the Nutrition Coalition Scientific Council. She’s also the medical director at Virta Health and together they have partnered to conduct the largest and the longest clinical trial looking at treating diabetes with a low carbohydrate diet and they’ve had such profound results that if this were a drug trial we would all be trying to buy stock.
Dr. Hallberg: My name is Dr. Sarah Hallberg and I’m a physician and medical director at the Indiana University Health Arnett medically-supervised weight loss clinic. I’m also the medical director at Virta Health, a remote care specialty clinic aimed at managing and reversing type two diabetes, utilizing a low carbohydrate diet. I am also Aspen Institute Health Innovator Fellow and I’m the chairman of the board of directors at to the Nutrition Coalition.
Emily: Hi Sarah. I’m so excited to talk to you.
Dr. Hallberg: Very nice to meet you.
Emily: Very nice to meet you too. If you want to talk a little bit about how you got into this field and how you sort of looked at this problem in a new way, that would be great.
Dr. Hallberg: Absolutely. So I had an interesting introduction into this field. Never in a million years would I have imagined myself here when I first went into medicine. So first of all, medicine was actually a second career for me. My first career was as an exercise physiologist and I had a master’s degree in that and worked for a while in that field before really finding out that can’t beat them, you have to join them basically when it came to positions in medical care that physicians didn’t have a great knowledge base when it came to lifestyle medicine, including exercise physiology and that I was just not going to get listened to unless I was a physician myself. So it was sort of that situation that caused me to go back to medical school after completing my master’s degree and working for a couple of years and then I had all intentions of going into preventative cardiology actually was my goal. But then since I was older, I wound up having a baby my first year in internship. So the first year after medical school and that moment in the delivery room completely changed my whole goal and I wound up stopping at internal medicine in practicing primary care just again so I could spend more time with then what became three children and I was in primary care for close to a decade and I really realized quickly on that I was just part of the problem and I was not really playing any role in the solution of what was clearly already in this has been obviously almost a decade and a half ago, this insurmountable problem of metabolic disease.
Emily: To interrupt you for a second. So tell me how did that happen? Like you, you’re seeing all these patients, I feel like there’s so many doctors out there who are in that same situation, but haven’t had that kind of an epiphany. How would you sort of explain that process?
Dr. Hallberg: I think that they probably have had the epiphany, but what has happened is they feel powerless and that is a really frustrating position to be in. And I felt that way myself. So in other words, we’re so pushed, right? You can spend 10 minutes with a patient and in there you’re supposed to deal with a list of eight problems, which is the general size of a problem list when you’re dealing with multiple metabolic diseases of a patient coming into your office. So you know you have to address their cholesterol, their high blood pressure, their diabetes, their obesity. And you’re doing all of this in this 10 minute window. So really what are you stuck with your stuck with prescribing more medications because that can be done relatively quickly and there’s no time to address the root cause of these problems, which is what are you eating? What is your diet like? Tell me what you’re consuming. And so again, you become a legal drug dealer and that’s always what I called myself. I’m like, I’m a legal drug dealer. I just write prescriptions. That’s all I do. And the system is set up to encourage me to do that at every level. Write a prescription for this, write a prescription for that. And I had what I felt at the time was a really good understanding of lifestyle medicine. Given my background and just there was no opportunity to do this. But then for me, I got a huge break in that Indiana University health came to me and asked me to start their obesity program and this was going to be a start from scratch program. There wasn’t one in existence at the time, so it really fell to me to say, what are you going to do? How do you solve this? Like air quotes, unsolvable problem, which is obesity in this country
Emily: And what year was that?
Dr. Hallberg: It’s been close to a decade now and so I had the opportunity because of that to literally get some time within a year period to go back to the books essentially and figure out what we were going to do. I read everything.
Emily: What an awesome opportunity to have that luxury too where you just get to go back to the research. I can imagine that was fun.
Dr. Hallberg: And so this thing is that when I was an exercise physiologist, what I was taught is that we should all be following a low fat diet. That was the nutritious thing. That was the key to health was removing fat from your diet and when I had that year, it was really quick getting into the literature and it struck me. There’s like no evidence for this. I’ve been saying this for a very long time because that’s what I was taught and that’s kind of what you take. You take it as it is, this is what you’re taught, this is what you learn in medical school. This is what I learned in graduate school, and to be slapped in the face, to realize the lack of evidence, to support that and understanding how it was failing huge in this country and across the globe as we see unprecedented skyrocketing of obesity and type two diabetes among other metabolic diseases. It was a real wow moment.
Emily: That’s partly because when you’re in med school, you don’t have time to go back to this raw data sets or original research. You’re just sort of given information and you’re quizzed on it. I mean, is that a fair assumption in why you had the time to go back and look at this research in a different way later in your career?
Dr. Hallberg: Yes, but it’s even worse than that because the fact of the matter is, despite the fact that no matter what specialty a physician goes into date are going to have to deal every day in and out with nutrition-related diseases. And guess how much nutrition is taught in medical school. Next to nothing. And so it’s crazy. Physicians come out and they’re unprepared. So if they have very limited nutrition, they’re told a couple facts, probably nothing that’s going to be all that important into translating any of that into their clinical care. And that’s all they have to go on. So you’re right, no time, but also incredibly limited information that they’re given school. So having that year, I really got mad cause I was like, wow, I’ve been coaching people and guiding people wrong and there’s gotta be a better way.
Emily: What were some of the things that you looked at that were the most upsetting to you? I mean, I could probably come up with a list that we would agree on, but it’d be great to hear from you what you sort of felt made you want to throw your coffee cup across the room.
Dr. Hallberg: So it was just that when we started pushing a low fat diet, when you go back and look at what literature was available there, nothing existed to support that. And the ruckus that was raised at the time, because there were a number of scientists saying, you know, this is not something that we have rigorous evidence for. This is essentially an experiment. And that’s really what it turned out to be. So there were a number of trials, like some of the Keys trials that people have cited as being the reason behind it. But when you look at what the quality of evidence was there, it’s minimum to none. And so it’s just a huge shift in what we were feeding an entire population based on scant evidence at best. So when I wanted to open the obesity program, I started out as a low carbohydrate intervention because there seem to be some promising research in that area. But what we saw happen so quickly is that our focus really turned away from obesity. Although obesity was improving, people were losing weight. We really hyper-focused on diabetes because we felt like this is the area more than anything where we were having the greatest impact and it was so rewarding. I just can’t even tell you how joyful an experience it is to like walk with our wonderful patients through a journey that restores their health. It is fantastic and it’s what gets me up and working every morning.
Emily: And since then, then you linked up with Virta and you guys have now done some of the only sort of clinical trials looking at the low carb diet. And just to backtrack for a second, it’s important for us to address the statistic, which I think you do a really good job of mentioning, which is that 50% of Americans are either pre-diabetic or diabetic right now and that it’s costing the country more than $3 billion dollars. That’s with a B a year in treatment. And that the idea that this is a disease caused by high blood sugar and we know that carbohydrates cause blood sugar to rise and the standard of care is to do insulin injections, which you’ve basically figured out you can get people off of by putting them on a low carbohydrate diet. Is that all fair?
Dr. Hallberg: Yes. And the cost associated with this are staggering. It’s actually $350 billion dollars and the rate is rapidly growing. It’s actually even one in three medicare dollars are spent battling this disease. So what if we could make a difference in this? I mean, what if we could actually make a difference in the disease process? Because once again, going back to standard of care is that this is a chronic and progressive disease. And I will tell you that I 100% reject that idea. It’s chronic and progressive only if you treat it with what has typically been the standard of care and then it becomes chronic and progressive. I mean the physiology just doesn’t allow for anything else to occur, but when you restrict the cause you restrict the carbohydrates. The physiology is on the patient’s side actually and disease reversal can occur, which includes medication reduction. And I was really fortunate to meet Dr. Steve Phinney, one of the founders of Virta Health at a conference told him what we were doing in Indiana and at the time I was looking for funding for a larger study and literally over dinner one night Steve and I had decided to partner on that trial on bringing Virta Health trial to IU Health and we ran an incredibly successful trial that as actually still ongoing, we’re about to start data collection 3.5 years into the trial. So it’s actually not the only trial by far looking at low carbohydrate diets in type two diabetes, but it is the largest and the longest and involves some really unique aspects of how do you implement a low carbohydrate diet actually aimed at achieving nutritional ketosis in patients with type two diabetes.
Emily: Okay, so just to clear up a couple of things. When you say low-carb, what do you mean? Like how many grams of carbs or how are you limiting it?
Dr. Hallberg: We see low carbohydrate that term tossed about all the time and so people will say low carbohydrate if the carbs are just under 50% of total caloric consumption, which if you talk to any expert in the field that is not low carbohydrate. So low carbohydrate really is for sure less than about 75 grams of carbohydrates a day. But in the world that I work in, we work more in very low carbohydrate, which is less than 50 total grams of carbohydrates a day. And for patients with metabolic disease that generally is even lower, less than 30 total grams of carbohydrates a day. Because our goal is actually to induce, again, a state of nutritional ketosis. And what that means is it’s essentially flipping your metabolism from burning carbohydrates exclusively for energy to actually utilizing fat, which is oxidized into ketones. And these ketones are brilliant fuel sources. And so nutritional ketosis is fantastic. Number one, again, taking away the carbohydrates which are causing glucose and insulin to go up. But number two, when we’re inducing the state of nutritional ketosis, we can be sure that that is the substrate that’s being utilized for energy in people. And that again contributes to the weight loss. And there are a lot of other exciting benefits that are being elucidated every day in regards to the state of nutritional ketosis as it’s being a powerful anti inflammatory agent among others. And so one of the things we always say to patients is pushing the vegetables, make sure you’re getting your non-starchy vegetables. And the rule is though never eat a veggie without fat. So I always like to tell my patients, imagine that vegetables are a vehicle for fat consumption. People can eat meat, they can eat eggs for sure, but it’s actually not required. I mean the other thing about low carbohydrate is this can be really conformed to any style of eating. So people, if they enjoy Mediterranean style of eating and that is so simple to do low carbohydrate. If people want to do a plant based diet, absolutely can be done low carbohydrate. It’s certainly not a strict meat and cheese meal and in fact really that’s one of the misunderstandings about it is that people presume then that it’s a high protein, therefore a high meat diet and actually it can’t be. So a well-formulated low carbohydrate diets aimed at nutritional ketosis cannot be meat-heavy and that is because you would be getting too much protein. Again, a well formulated ketogenic diet is low carbohydrate, moderate or we like to say adequate protein and what’s high, it’s the fat content that’s high.
Emily: Can you give me a breakdown of what that looks like? So it sounds like it’s like about 30 carbs, net carbs a day or grams of carbs a day.
Dr. Hallberg: Total carbs a day. And that’s where we start people and then we personalize it, which I’ll get into in just a minute, but like what would a typical day look like? So let’s start off for breakfast. I mean breakfast can look like full fat Greek yogurt with maybe some nuts or even some berries depending on their carbohydrate tolerance. But it’s good just to put like a little bit of peanut butter in a full fat yogurt that’s a quick and easy breakfast enjoyed by many of our patients. You certainly could have eggs or even bacon. We would encourage you know, something to be added with that additional fat or possibility even vegetables, so many patients will enjoy like spinach and eggs in the morning is another great way to start the day. And certainly some people enjoy making low carbohydrate muffins ahead of time and they can have that with some butter on it in the morning. So you know, breakfast can look like those are just three examples. There are even low carbohydrate pancakes that are just amazing that are eggs and cream cheese with a little bit of cinnamon. They’re just out of this world. So there’s just so many varieties just alone for breakfast. And then lunch, I mean our typical patient I think which is typical in America in general is that people will eat salads and of course we would say you know, heavy on the olive oil and they can utilize some other dressing as well. But we would always encourage additional olive oil to be added to that. Of course they could still have something like, there’s plenty of soups that they could have for lunch, you know, salmon or a small piece of meat if they would prefer. A lot of times people will have leftovers from the night before and dinner is the most endless possibility ever. So many different things from casseroles to.. In our house we utilize the instapot is all the rage in my household because we can make stews and roasts and all kinds of things in that very quickly and easily. One stop shopping and we always have lots of vegetables, we’ll have a salad and a vegetable at dinner in addition to some source of protein. So first thing is we start, we never ever, and you know, this is absolutely true at Virta Health and in the study and in our everyday patients that we treat at Virta is we never tell someone what to eat. We want to educate them. And so when you get back to this basic physiology, I mean the basic physiology is so easily digestible. We have three macronutrients. It’s fats, proteins and carbohydrates. Insulin is our fat storage hormone. Carbohydrates cause glucose and insulin to rise. That is a big problem. Fats don’t cause a rise in glucose or insulin. And so if we go back to this concept that we’ve been taught for so long that a calorie is a calorie and the calories are all that matters, it defies the hormonal reactions to these macronutrients. And you just can’t do that. You can’t constantly work against your hormones, essentially is what we do with a low fat diet and expect success. And so we need to have and help people understand that basic physiology, and I always say humans, we are all different and that is so important in personalization of any lifestyle recommendation, but there are things that are just human. And again, our reactions to these macronutrients, the facts that carbs cause glucose and insulin to rise in everyone maybe to different degrees, but in everyone and fat is that flat macronutrient. That’s part of human nutrition physiology. And so again, getting them to understand that, and you’re right, divorcing people from the idea of counting calories is at the exact same time freeing and liberating and terrifying because we really have to, I mean it’s cognitive dissonance, right? I mean that’s it and I like to call it what it is. This is cognitive dissonance. This is fighting against what you’ve been told all this time. But let’s go through these basics. Let’s understand why what we’ve been told doesn’t make sense. There’s just the basic science behind it doesn’t make sense. And people leave and go, oh my gosh, and you get, we get reactions when you really go through the basic physiology from total anger to actually tears. Sometimes when people are like, oh my goodness, I get that. That makes perfect sense. But then what happens is a month, two months, three months down the line again, those old habits, the old ideas, you kind of have to remind people and you know, going back to the days in primary care when I was a legal drug dealer, now when we’re talking about medication management, we’re talking about Virta and the experts in de-prescribing. Which is just so fun to do. To tell someone, hey, you know what? Today is the day you get to stop your insulin. You know, even to people who have been like, I can’t believe it. I’ve been on insulin for 20 years. Well that was 20 years, but tomorrow’s a new day and you will start the day without it.
Emily: They must have such a positive response to that news. I can’t even imagine what that’s like.
Dr. Hallberg: It’s just such an honor to be with people when you get news and you get to celebrate milestones like that and we get to do it a lot. For example, I’ll tell you in our clinical trial, at one year, 94% of the patients who started the trial on insulin had their insulin decreased or totally removed. And then people will say, well wait a minute, that’s only a year. Well guess what the numbers were at two years? 93%. So this is not only making those improvements but sustaining those improvements over the long haul.
Emily: And do those people then stay in the study? Like you’re going to continue to follow them for years and years? Or is it, is that done?
Dr. Hallberg: No, it’s ongoing? So we’re just about to do three and a half year data collection and it will go out to five years. So you know, we’re in this for the long haul and we’re interested again in seeing these remarkable results and sustaining these remarkable results. So that is very exciting to be a part of.
Emily: And so will you just talk a little bit about what you do when somebody enters the trial or like for somebody who might be listening who’s diabetic, obviously I’m not a doctor, I can’t give any advice. But in terms of what you guys are doing, you’re not just saying like, okay, just you know, don’t take your insulin and just eat a low carb diet. Like it’s very regimented, right?
Dr. Hallberg: And it’s very education focused. So when someone starts at Virta Health, they meet their health coach, they meet their physician, they actually get a kit of everything that they’re going to need. A cell phone enabled scale, ketone monitor, blood sugar monitor, blood pressure cuff if needed. Everything they’ll need to succeed. And then when they meet their health coach and they set a date for them to get started. But important to note, set a date, right? So we don’t have anyone just jump into this because there’s actually like a pre-planning period. Like what’s in your kitchen, you know, we need to get, we need to get it stocked with the right things. We have to set people up for success. So stage one if you will is let’s prepare your environment. What do we need to have, what do we need to make sure we don’t have? What kind of discussions do you want to have with family? Who are you going to involve in this? Who is your support people? Who are going to be your accountability partners? Of course we’re providing accountability partners, especially through the health coaches, but who are the accountability partners in the home or in the workplace? So those kinds of preplanning things. And then getting started after the education pieces have been in place with learning how to limit carbs. And again, the health coach will be, how did you do today? What did you have for breakfast? And they’re making these recommendations personalized because they’re reacting to biomarkers that the patient is entering. In other words, you know, if their blood sugar dropped significantly, hey, what happened last night for dinner? Because it went really well. Your blood sugar dropped this morning. If it didn’t drop and we expected it to, let’s go back and look again at what dinner was. So we’re able to make recommendations almost in real time. So it’s not like you go into your doctor’s office in a month and you’ve lost two pounds. Well, what worked and what didn’t during that month period because we’re attaching it right away.
Emily: And do you find that the sort of the range of nutritional ketosis through those blood glucose monitors, is there like a sweet spot that you guys really like that people could look for if they were testing their fingers at home?
Dr. Hallberg: As a general rule, we look for 0.5 millimoles beta hydroxy butyrate via a finger stick. And that is actually based out of the work from Dr. Steve Phinney and Dr. Jeff Volek where we seem to see most of the advantages of nutritional ketosis take place. But there is clearly some person to person variability. In other words, there are people who are just hitting a home-run in inflammation markers, diabetes reversal, and they tend to be around 0.3 and there are certainly people who are finding great deals of success who are higher than that. So again, that’s one of the advantages of having a health coach and physician because we can help watch a person’s individual response and make carbohydrate and ketone goals accordingly.
Emily: And so one of the other things that I feel like I have to ask because another pushback that I often hear on the sort of low carb lifestyle or that sounds strange, but is the idea of kidney failure, right? Or like kidney damage, which it seems like people are really hung up on that idea that you can destroy your kidneys on a low carb diet. Is there any evidence to support that idea?
Dr. Hallberg: So here’s where that came from. Like why did that, why is that even a thing? Like why didn’t anybody think of that? And really that dates back to when low carbohydrate was perceived as a really high protein diet. And protein and kidney function is a really hotly debated area in nephrology or kidney specialty. How much protein do patients with chronic kidney disease, how much should they be consuming? I’ll leave that to them to debate. The thing is that a well formulated ketogenic diet is never high protein and so it’s kind of a moot point. And again, if you look at the studies and the data on this, we don’t see a negative impact on kidney function. So there’s just, there’s no evidence to support that notion at all.
Emily: Now you just recently went before Congress and presented the results from your study and I assume some of this sort of educational piece. I can only imagine what that was like in terms of going before the people who are recommending the standard American diet or even supporting the American Diabetes Association recommendations. How did that all go? What was that experience like for you?
Dr. Hallberg: It was great actually and I think interestingly members of Congress are interested. They realize that we’re in big trouble and they’re interested in changing. I think that there has been some paralysis in doing that which I hope we will be able to overcome. There certainly is, though, interest. And on standard of care and the American Diabetes Association, I want to share some really exciting news and that is that in the 2019 Standards of Care in Diabetes, which comes out every year, it’s essentially the American Diabetes Association guidelines. For the very first time, they acknowledged low carbohydrate diets as a recommended eating pattern. So for the very first time they are a recommended eating pattern and they went further to say that low carbohydrate diets are the eating pattern that shows evidence for disease reversal, although they did not call it disease reversal, they acknowledge the ability to decrease medication, which is of course reversing the disease process.
Emily: My immediate inverse question is going to be what about prevention? I mean when we’re talking about kids, I’m in the process of trying to get the sugar out of my kids’ cafeteria and one of the things that I’ve gotten push back on is that the parents get really upset when the chocolate milk is taken away or when the desserts on Friday are taken away. And I find that to be so interesting and some of the parents that I’ve talked to candidly about it will say things like, oh well, you know Johnny’s so skinny. I can’t get him to eat anything. And so I have to give him this crap because it’s the only thing he’ll eat and I wish that somebody could, and I’m hoping that you can sort of articulate how this is a cumulative problem. People don’t start out with this, that it develops because your body becomes metabolically incapable of processing the sugar. Is that correct?
Dr. Hallberg: Yeah, I mean it floors me. It just floors me that parents are not universally embracing this. I think we have a lot of parents who are getting it more and more. But I mean if I could tell you how many patients in my clinic the same story, I was a thin kid, I never had to worry about this before. This is new to me. Just because you have a thin child doesn’t mean you can let down and let them eat sugar all the time. And that’s exactly what we do because they’re getting sugar in all these different ways. Every reward, every treat. It’s just sugar and sugar and sugar and we send them off to school. It’s cereal, you know, which is again just sugar and we say, oh, it’s great because this is whole grain cereal. Really. You’re just giving them a huge carb load in the morning and then you’re putting your low fat milk in it, which is just more sugar in. It’s more and more and more. And so what I tell parents is only goodness, this is so important to start as a family. Now, low carbohydrate for kids can be very different than it is for an adult with metabolic disease. I mean, I consider my children to be low carbohydrate kids. That doesn’t mean they never have sugar. It means it’s not something that’s in our house and I have to deal with it. They’re going to get it when they leave our house at times and I can accept that. But in our house they get protein and vegetables and they start off their day. I mean my kids like eggs and they start off their day with eggs and I make sure they have plenty of fat and protein in the morning. And I always tell parents, say if there’s one thing that I could do, because I get that question a lot and that is a really easy to answer question. If there is one thing you could do, never, never give your kids juice or soda. No, not sometimes. Not because it’s a vacation, not because you’re taking them out to a special dinner. Juice and soda are nevers for all children. There’s no reason that there is nothing beneficial about those with kids. And so if parents could just take that one single step to never let their kids have juice and soda, I mean that would be a huge first step.
Emily: I’m in complete agreement. I feel like we tell our kids when they go to birthday parties that they can have cake or juice. That’s sort of the choice they get to make when they’re at a birthday party. But I think people think we’re terrible. You know, like we’re so mean for doing that.
Dr. Hallberg: Well juice is good for you, right? People think. And actually if you look at it. It’s worse than soda. It’s like a sugar bolus. It’s like an IV sugar bolus.
Emily: That was Dr. Sarah Hallberg who I feel like opened all of our eyes to this idea that if you’re diagnosed with a chronic disease it does not mean that you’re going to die of the chronic disease. There are certainly things you can do about it and in her clinical trial where they’ve reversed 60% of diabetes in the people who were in the trial I think is going to be a landmark study. We’re all going to look back on. Some of the big takeaways for me were the fact that the cholesterol in these people who participated in the study were not negatively impacted. That kidney function is not negatively impacted by a low carb diet. That giving kids sugar for breakfast is setting them up for failure probably in terms of academic success as well as in terms of their overall health and that this is a cumulative problem. So even if your kid is skinny and has lots of energy and doesn’t like to eat food, giving them the wrong food is going to make them sicker sooner. And obviously that’s not something that any of us wants. When Dr. Hallberg said that the American Diabetes Association had changed their guidelines to include a low carb option for diabetics, it was the first I had heard of it. I was pretty shocked because I feel like that would mean that the Virta study has already had a massive impact on the sort of established way of treating diabetics. I was curious what Dr. Gabbay would say about this addition and the ADA guidelines. And sure enough, he has a slightly different take on it. Here he is.
Dr. Gabbay: The American Diabetes’ already sort of come out this year with a more flexible approach to diet. It includes potentially lower carbohydrates but not a– low carbohydrate can mean a lot of different things. The version that was sort of the advocate is extremely low carbohydrate and ketosis and there are some concerns about the safety of that for all people with diabetes. So that’s not what the ADA’s come out behind?
Emily: Okay. And so from your research and your experience, you know, when you have you had a chance to look at any of that?
Dr. Gabbay: Sure. Oh yeah, absolutely. Yeah.
Emily: And so what do you think, what do you make of that?
Dr. Gabbay: I think there are some patients that can benefit from that. Absolutely. I might make some more general comments about diet. When most diets are compared to each other, so for example, for many years it was the advocacy was really around low fat and then over the last several years to lower carbohydrates. When you do studies that compare one to the other, they’re pretty much equivalent. It’s difficult to show a big difference. And the reality is in each group, there are people that do extremely well and then other people that don’t do well at all. And so what I take from that is that, it sort of depends on the person. For some people, their best strategy for losing weight is going to be cutting carbohydrates. For some people it’s going to be cutting fat. The ideal is people meet with a nutrition specialist that helps to guide them on that. But I’ll often ask patients have you ever tried to lose weight? Have you ever been successful? And what worked for you? And people often know what works. A and that probably is the best predictor.
Emily: You see, I feel like one of the things that I was, and I’m sure you know this, but like they say that they had 60% of their subjects reversed diabetes and 94% of their subjects were off insulin altogether or reduced their intake of insulin. So that doesn’t seem like some people, right? I mean, that’s the majority of the subjects in their study. Yeah.
Dr. Gabbay: You know, there may be some caveats with that. You know, it’s A. not necessarily all [?}, maybe a somewhat selective group. It requires a pretty significant ability to adhere to something that not everybody’s willing to do. And so you know, another way to frame that is a there are a variety of different intensive programs to lose weight and people that follow those programs can do extremely well. The question is what percentage of people are those?
Emily: Dr. Gabbay’s point that there’s a connection between obesity and diabetes and that that’s probably the biggest risk factor and essentially getting the weight off any way you can is beneficial is definitely how people have traditionally thought of this. But there is another school of thought that thinks of this as a hormone disregulation within the body and there’s some research out by Nuttall and Gannon and we’re going to link to it on our site. They have a series of well-designed controlled experiments where they’re demonstrating that carb restriction is effective in treating diabetes under conditions where no one lost weight. That’s really significant, right? Because that basically means they are regulating the hormones by removing the spikes in insulin even though the subjects aren’t losing weight. So I think there’s sort of two schools of thought on this. The way that Dr. Hallberg talks about it, she’s basically saying, hey, if you get rid of the carbs and you don’t have these spikes, then the body’s sort of not in shock and it can manage better. Whereas when you’re eating a low calorie diet, you could be eating a low calorie diet of say peeps, and that’s all sugar, right? So you’re just constantly spiking your system that could make you diabetic or prediabetic. So I think that’s really interesting. Okay. To wrap up, we’re going to also hear from Dr. Gabbay about the idea that Joslin has been treating people with diabetes on a modified low carb diet for a long time.
Dr. Gabbay: We’ve been doing that for a number of years. Not to the extremes of developing ketosis as their work has been, but absolutely we’ve been early adopters and rolling back some of the historic recommendations of the American Diabetes Association and in part some of our studies that have shown long term weight loss for a program we have here has helped to sort of identify, yup, there’s a rationale for lowering carbohydrates and not being at sort of 60% which at one time was the sort of standard recommendation.
Emily: Dr. Gabbay made some good points. I think it’s important to mention that this was not a randomized double blind controlled trial, meaning that people weren’t just randomly picked and then tested in a way where they didn’t know which diet they were on or that you’ve took one group and fed them one thing and the other group, the other, and then you could compare. However, I think given the fact that they got the results that they did with 60% of participants reversing their diabetes and 94% of participants eliminating or reducing their insulin. This is still incredibly significant and so you can be hard on the rigor of the study, but I actually don’t think that that takes away from it too much, but it’s an important point. I also thought it was really interesting that he sort of seemed to say the most important sort of risk factor for diabetes for probably developing it and for treating it is being overweight and that if you lose weight on a calorie restricted diet, that’s great. If you lose weight by eating ad libitum and you’re on a low carb ketogenic diet, that’s fine too. That the point for him seems to be really, you got to get the weight off and then the sort of more nuance takeaway for me was when he said that Joslin was an early adopter of the low carb recommendation because I don’t know that he would have said that five years ago. I wonder whether the Virta trial is now opening people to this idea that low carb is a way of treating diabetes and making it more of a thing that conventional sort of established medical systems are saying, oh yeah, we’ve been doing that too, because now the door has sort of swung open. So I don’t want to leave you all without going back to Kim and hearing how she’s doing. So here’s Kim. So will you just give me a rundown of what medicines you were on before that you are no on.
Kim: I was on Toujeo 38 milliliters. I was on 10 milligrams of Glipizide. I was on 2000 milligrams a day of Metformin. I was on three blood pressure medicines. I don’t even know that I could name all three of those. We’ll just say three blood pressure medicines. I was on 80 milligrams of Omeprazole for GERD. I was on an iron pill. I no longer have to take that. The only things I’m on at this point is I still take a blood pressure pill and I’m going back to Dr. Hallberg for my three and a half year checkup and we might discuss that. So I’m hoping to be able to dump that. But if I can’t, that’s okay. And I would take Tylenol for arthritis. I was on arthritis medicine as well, prescription arthritis meds. And that’s fantastic. And I may be missing something. I didn’t count how many of those are, but I know it was ten so technically I’m only on one prescription med at this point. And that’s for blood pressure.
Emily: And how are your numbers? How have they changed?
Kim: Well, I’ve gone from 268 fasting to this morning. I was at 105
Emily: So if you could go back in time and tell yourself what you now know, what would that experience be like?
Kim: I would have eaten butter. How’s that?
Emily: There’s something so profoundly upsetting and just as exciting about Dr. Hallberg’s research and the fact that everything that we’ve been taught basically about what we eat might be wrong and that it’s actually making us sick, but that those sicknesses aren’t things that we have to live with. That we can reverse them by simply correcting what we’re eating, eating more fat, eating less sugar, and that we can do this as a family and improve the future generations ability to live longer, healthier lives. I’m Emily Kumler and that was empowered health. Thanks for joining us. Don’t forget to check out our website at empoweredhealthshow.com for all the show notes, links to everything that was mentioned in the episode as well as a chance to sign up for our newsletter and get some extra fun tidbits. See you next week.
Emily Kaplan is an expert in strategy and communication. As the CEO and Co-founder of The Broken Science Initiative, she is building a platform to educate people on the systemic failings in science, education and health while offering an alternative approach based in probability theory. As the principal at The Kleio Group, Emily works with high profile companies, celebrities, entrepreneurs, politicians and scientists who face strategic communication challenges or find themselves in a crisis.
Emily’s work as a business leader includes time spent working with large Arab conglomerates in the GCC region of the Middle East looking to partner with American interests. Emily acquired Prep Cosmetics, expanded it to become a national chain and revolutionized the way women bought beauty products by offering novel online shopping experiences, which are now the industry standard. She was a partner in a dating app that used the new technology of geolocation to help interested parties meet up in real life. Emily developed Prime Fitness and Nutrition, a women’s health concept that focused on the fitness and diet needs of women as they age, with three physical locations. She was the host of the Empowered Health Podcast, and wrote a column in Boston Magazine by the same name, both of which focused on sex differences in medicine.
Emily is an award winning journalist who has written for national newspapers, magazines and produced for ABC News’ 20/20, Primetime and Good Morning America. She is the author of two business advice books published by HarperCollins Leadership. Emily studied Advanced Negotiation and Mediation at Harvard Law School. She has a Masters of Science from Northwestern University and received a BA in history and psychology from Smith College.
Support the Broken Science Initiative.
Subscribe today →
One Comment
Comments are closed.
recent posts
And more evidence that victory isn’t defined by survival or quality of life
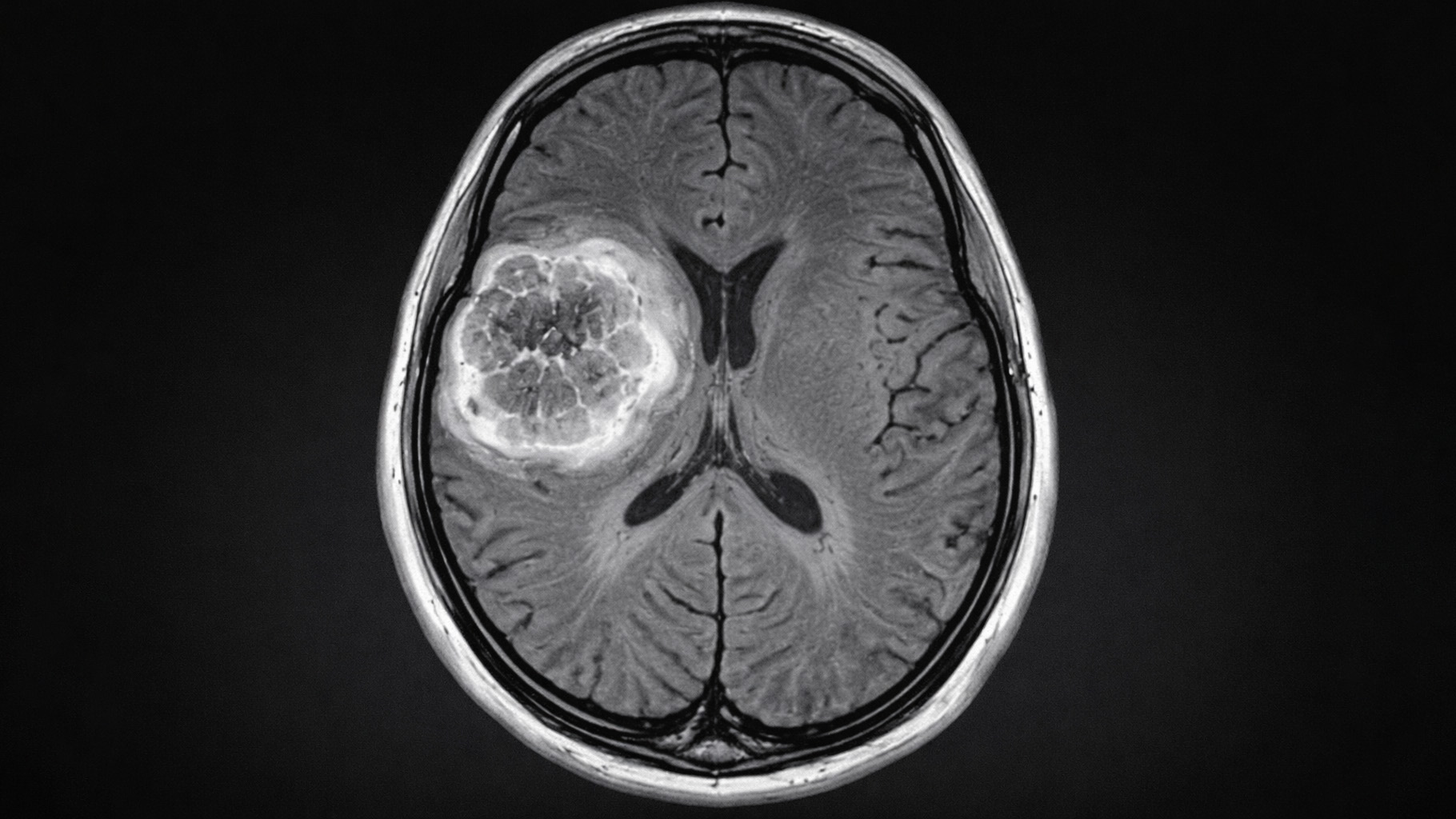
The brain is built on fat—so why are we afraid to eat it?
Q&A session with MetFix Head of Education Pete Shaw and Academy staff Karl Steadman

[…] objectivity? Like this is so compelling. How come this isn’t getting more press than when we interviewed Dr. Hallberg for the podcast, the person who helps them with public relations stuff followed up with us a couple times and was […]