In Part 1, we explored how fasting and feeding influence energy metabolism, particularly the body’s reliance on carbohydrates and fats for fuel.
Brief recap:
- When we eat, insulin rises, promoting glucose uptake and shifting metabolism toward carbohydrate oxidation, while fasting lowers insulin, increasing fat oxidation and eventually leads to ketone production when fasts extend beyond ~16-24 hours (largely dependent on how active we are!).
- While time-restricted eating (TRE) can be a useful tool for weight management, preserving muscle mass requires resistance training and adequate protein intake.
- Fasting alone does not appear to induce mitochondrial adaptations in human muscle, contradicting common assumptions about its role in improving metabolic flexibility. Instead, its metabolic benefits may be more tied to caloric restriction rather than direct improvements in muscle metabolism.
In this article, we discuss what happens when we pair fasting with exercise.
Fasting is one thing. Exercising while in the fasted state is another.
Let’s first address the metabolic differences when we exercise in the fasted state compared to the fed. For this article, fasted exercise refers to the overnight fasted state, as in you wake up, workout and then eat.
Fasted vs. Fed Exercise Metabolism:
In the fasted state, fat oxidation is prioritized due to lower insulin levels and elevated glucagon and catecholamines (epinephrine). This promotes the release of fatty acids from adipose tissue (lipolysis), increasing free fatty acid (NEFA) availability and oxidation. Essentially, you have more fat available for fat oxidation because carbohydrate availability is lower.
In the fed state, the relative proportion of fat to fuel substrate utilization is reduced and carbohydrates increased. Consuming carbohydrates before exercise increases insulin, suppressing lipolysis and reduces NEFA availability, leading to greater reliance on blood glucose and muscle glycogen. So, because carbohydrates are available, we burn more carbohydrates.
The graph below shows fuel substrate utilization during exercise of different intensities between the fed (550 cals; 87% carbs) and fasted (12-hr overnight fast) states, as well as between trained (cyclists) and untrained (<2 hours of physical activity/week) young males.
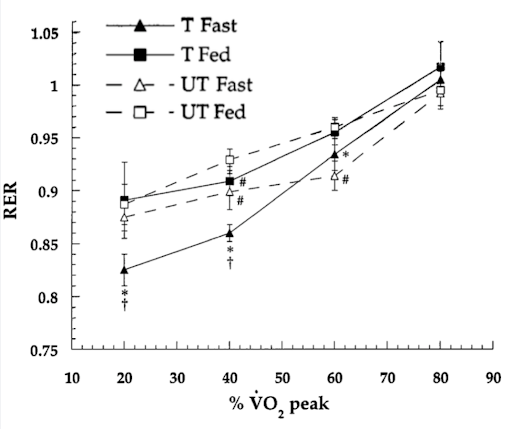
Source: Bergman & Brooks, 1999: Respiratory gas-exchange ratios during graded exercise in fed and fasted trained and untrained men. Journal of Applied Physiology.
There are a couple takeaways from this study:
- Regardless of if you are trained or untrained, fasted exercise results in lower RER (higher fat oxidation) during moderate intensity exercise (somewhere above 22% and below 75% VO2peak), but if you are trained, this difference is seen even during very low-intensity exercise (22% VO2peak)
- Somewhere above 59% VO2peak, it doesn’t matter if you are in the fed or fasted state, carbohydrate dominates fuel substrate utilization and training status doesn’t change this.
The suppression of fat oxidation by pre-exercise carbohydrates during moderate-intensity exercise is a consistent finding within the fasted vs fed exercise literature (Vieira et al., 2016).
But why wouldn’t metabolism be different between the fed and fasted state at high exercise intensities?
Well let’s take a step back and consider fuel sources during exercise.
The two primary substrates are carbohydrates and fats with the four primary sources being blood glucose and muscle glycogen for the former, and free fatty acids and intramuscular triglycerides for the latter.
Exercise intensity dictates not only substrate type but substrate source.
Fuel Substrate Utilization During Exercise Across Different Intensities
- Low-Intensity Exercise (~25% VO₂max; think brisk walking)
- Primary fuel: Fat oxidation, predominantly from circulating free fatty acids released from adipose tissue.
- Carbohydrate contribution: Minimal, with a small increase in blood glucose uptake.
- Intramuscular triglycerides (IMTG): Little utilization at this intensity.
- Moderate-Intensity Exercise (~65% VO₂max; what you could sustain comfortably for a couple of hours)
- Primary fuel: Fat oxidation peaks, with equal contributions from fats released from adipose tissue and IMTG.
- Carbohydrate contribution: Increases significantly, with both blood glucose uptake and muscle glycogen utilization rising.
- Metabolic shift: This intensity represents the crossover point where carbohydrate oxidation starts becoming more dominant.
- High-Intensity Exercise (>85% VO₂max; exercise you cannot sustain for very long)
- Primary fuel: Carbohydrate oxidation dominates, primarily from muscle glycogen, with some contribution from blood glucose.
- Fat oxidation: Declines due to metabolic limitations, including reduced circulating free fatty acid availability and restrictions on mitochondrial fatty acid transport.
- Energy demand*: Rapid ATP resynthesis favors glycolysis, leading to increased lactate production.
*This is why it doesn’t matter whether you’ve eaten or not before high-intensity exercise, because the metabolic demands are so great and the source of fuel is locally within the muscle (muscle glycogen). So the impact of insulin on circulating fuel availability doesn’t matter. Since muscle glycogen doesn’t budge while we fast overnight, pre-exercise carbs don’t make a difference to starting glycogen levels (that is, if you’re fed or fasted you have access to the same amount of muscle glycogen).
Other factors that influence fuel substrate utilization:
- Exercise duration: Over time, fat oxidation increases while carbohydrate oxidation declines as glycogen stores deplete.
- Training status: Well-trained individuals have greater fat oxidation capacity and glycogen-sparing adaptations.
- And previously discussed, Nutritional status: Carbohydrate ingestion prior to exercise reduces fat oxidation and increases carbohydrate use, particularly at moderate intensities.
What about adaptations to exercise, does it matter if we’re fed or fasted?
Fasted exercise is a “train low” strategy thought to drive greater endurance adaptations that make us fitter and better athletes. Those same adaptations are what result in greater insulin sensitivity, ability to burn fats, and ultimately, metabolic health. So, could fasted exercise give us greater health benefits? The average person only allocates so much time to exercise, and I think we are all interested in getting a better bang for our buck.
Training in the fasted state – that is waking up, getting your workout in, and then eating breakfast – does appear to have some advantages.
In sedentary overweight men, after 6-weeks of exercising before breakfast compared, insulin sensitivity only increased in the group that delayed breakfast until after their workout (Edinburgh et al., 2020). This was an interesting study that showed the more fat burned during each bout of exercise was related to the improvements in insulin sensitivity. And importantly, this study demonstrated that you could be following physical activity guidelines and not be getting health benefits from exercise if consuming a high carbohydrate meal before your workout. This is a bit provocative, but very interesting.
Similar results were reported when healthy men were subjected to a high calorie diet for 6-weeks but one group exercised before breakfast and the other after breakfast. Improvements in insulin sensitivity, resting muscle glycogen levels, and capacity to burn fat during exercise increased to a greater extent in the fasted exercise group (Van Proeyen et al., 2010).
Further, after 3-months of training in the fasted state compared to after a carbohydrate-rich breakfast, those who exercised fasted had greater improvements in HbA1c, independent of fat loss or changes in fat oxidative capacity (Verboven et al., 2020).
So, what I take away from this is that for those who are overweight and/or at increased risk for type-2 diabetes and/or with type-2 diabetes, fasted exercise may benefit from doing at least some of their moderate intensity exercise in the fasted state – independent of caloric intake.
I emphasize moderate intensity exercise because in overweight insulin resistant females engaging in a high-intensity interval training protocol, fasted exercise didn’t have any advantage over the breakfast-fed group for muscle adaptations or insulin sensitivity (Gillen et al., 2013).
In healthy males, six weeks of fasted training can also lead to a glycogen sparing effect during exercise (Van Proeyen et al., 2011) – suggesting fasted training can improve our ability to burn fats during exercise and may represent a legitimate tool for augmenting adaptations to moderate intensity endurance training.
There are a handful of acute exercise studies that show restricting carbohydrates around exercise results in a greater signaling response (the signal that precedes adaptations to exercise) (Stocks et al., 2018; Akerstrom et al., 2006; Guerra et al., 2014). So, it’s possible that there is an advantage to fasted over carbohydrate-fed exercise for augmenting endurance adaptations.
Where the waters muddy is when we fail to consider the population at hand.
Are you an endurance athlete training 10+ hours a week at risk of low energy availability? A legitimate concern with fasted training is that it can dig a caloric deficit hole early in the day that is hard to climb out of leading to chronic low energy availability and the symptoms of such (poor sleep, reduced recovery, suppressed immune system, etc.).
Does working out in the fasted state make you feel sluggish or nauseous? Are you not getting as much work done because you have no fuel on board? Then fasted exercise is probably not for you!
I think there is real science to suggest manipulating carbohydrate availability through fasted training can lead to some beneficial outcomes for health and adaptive outcomes. But, there is still so much to learn about how we can apply fasted training and to which populations it makes the most sense.
As a PhD candidate in muscle physiology Kristi Storuschuk’s research has focused on the interplay between nutrition and high-intensity exercise.
Support the Broken Science Initiative.
Subscribe today →
recent posts
And more evidence that victory isn’t defined by survival or quality of life
The brain is built on fat—so why are we afraid to eat it?
Q&A session with MetFix Head of Education Pete Shaw and Academy staff Karl Steadman