The caricatures, stereotypes, and tropes regarding getting old are plentiful and everywhere in the media, culture, and medicine. Dad noises, dated opinions held, mental decline, physical decline, and more are all representational constructs about the elderly and are present in all aspects of life.
Dad noises and physical decline are two related stereotypes that do have at least a foot in truth. How so? They overlap onto the concept of pain and the epidemiology of pain with age.
Pain is a constant companion throughout the life span. Although far less researched than pain in the aged, about 30% of teenagers report some type of recurrent pain (Gobina et al, European Journal of Pain 19(1): 77-84, 2014). In respect to older populations specifically, more detailed and numerous investigations clearly demonstrate that the incidence of pain is much higher with each passing decade:
| Age | % Reporting Pain | % with Althragia* (any joint) |
|---|---|---|
| 40s | 49.7% | 36.7% |
| 50s | 60.9% | 50.7% |
| 60s | 63.5% | 54.6% |
| 70s | 65.9% | 55.3% |
* Althragia = joint pain
(data adapted from Thiem et al, PLoS One 8(4): e67053, 2013)
In the data for the above table, the knee was the primary joint affected, accounting for 31.4% of reported pain incidences. Pain at the hip accounted for 15.6% pain experienced and reported. Another study found that each year 25% of those over 55 years of age will report having persistent knee pain. Within those numbers, 2.5% of over 55s experience consistent pain leaving those individuals “severely disabled” (Peat et al, Annals of the Rheumatic Diseases 60: 91-97, 2001). Further, an insightful and rather unique paper suggested that in older populations joint pain exists in two differing forms: transient intermittent pain and persistent background ache (Hawker et al, Osteoarthritis and Cartilage 16: 415-422, 2008). Determination of how each pain type is provoked has yet to be elucidated.
If about 60% of those over forty years of age report current episodic pain, with nearly 50% reporting some level of joint pain, this is an important epidemiological issue. How do we, how can we, lower pain perception or eliminate it?
Suspected causes
Before we start treating it, we might need to identify the causative agents for pain in older individuals. Causation data is hard to come by as nearly all modern research investigates correlations between variables and phenomena. This means that we can point to likely causes of pain but we cannot say absolutely, without caveat, that variable x, y, or z induces the pain that the elderly experience so commonly. As such, the sources of pain are generally attributed to diseases or syndromes of related symptoms due to similarities in patterns of occurrence.
The first, most commonly attributed potential source of pain in the elderly is arthritis (osteoarthritis). Osteoarthritis and joint disorders have been suggested to account for 82% of diagnoses in a fairly large study (St. Sauver et al, Mayo Clinic Proceedings 88(1): 56-67, 2013). If we consider a single joint, the hip, we find data that osteoarthritis of the hip affects about 11% of all adults across the life span (Fernandes et al, Annals of Rheumatological Disorders 72(7): 1125-1135, 2013). In another study, of the 15.6% of over 55s with hip pain, 10% of the total subjects were diagnosed with hip osteoarthritis, leaving 5.6% of cases resultant from other factors (Peat et al, Annals of the Rheumatic Diseases 60: 91-97, 2001). Osteoarthritis is a predominant but not the exclusive likely cause.
While it is stated that osteoarthritis is incurable (other than joint replacement) (Fransen et al, Journal of Rheumatology 29: 1737-1745, 2002), there are a few very common conditions that are related to osteoarthritis and pain. For example, it has been noted that any significant level of obesity is related to increased pain (Glei et al, Journal of Aging and Health 34(1): 78-87, 2021). Such a correlation may indicate that there is a link between derangement of metabolic status and osteoarthritis and its related pain. We can look at some representative data:
23% — Percent of the population that have physician diagnosed osteoarthritis
43% — Percent of the above 23% affected with prescribed activity limitations
49% — Percent of population with heart disease AND osteoarthritis
55% — Percent of the above 49% affected with prescribed activity limitations
47% — Percent of population with diabetes AND osteoarthritis
54% — Percent of the above 47% affected with prescribed activity limitations
31% — Percent of population with obesity AND osteoarthritis
49% — Percent of the above 31% affected with prescribed activity limitations
(Barbour et al, Morbidity and Mortality Weekly Report 66(9): 246-253, 2017)
It is apparent that the interplay between diet, exercise, and obesity driven metabolic dysfunction is a strong candidate for being the culprit in not only diabetes and heart disease, but also osteoarthritis and experienced pain. We know that we can reduce or eliminate obesity through diet and exercise. So, can we reduce pain and/or the frequency or severity of osteoarthritis if we do? This would be an exceptional outcome for those with pain and activity limitation.
Effects of diet and exercise on pain and osteoarthritis
There are literally dozens of methods to assess pain, most being simple generic Likert scales where the individual is asked to rate their pain on a scale between 1 and 5 or 1 and 10. There are others that that evoke a specific set of pressures on the skin and have the individual describe the severity of discomfort or pain. There are others with very specific populations and diseases in mind, such as the Western Ontario and McMasters Universities Osteoarthritis Index (WOMAC) which, as its name implies, is intended specifically to assess pain from arthritis (Bellamy et al, Journal of Rheumatology 15(12): 1833-1840, 1988).
Commonly used in older populations as they have much higher incidences of osteoarthritis than younger populations, one relatively weak study showed WOMAC pain score lowering by 2.4 units with a diet and exercise driven loss of 8.2 kg (18.1 lb). In this study, the faux “control” group (which received an educational intervention but did not receive programmed diet and exercise) had a 1.9 unit reduction in WOMAC score coupled with a -3.4 kg loss in bodyweight (Messier et al, Journal of the American Medical Association 328(22): 2242-2251, 2022). In a different study of older individuals (69 years on average), those who dieted and exercised moderately lost about 8.3 kg versus a loss of 0.1 kg in those who did not (control group). The weight loss group’s WOMAC pain score fell by 11.2 units while the pain score in the control group decreased by 1.7 units (Miller et al, Obesity 14(7): 1219-1230, 2012).
As indicated above, younger populations, up to about 30% of them, report periodic or consistent pain. However, unlike in older populations, adolescent obesity does not seem to be related to an increase in joint pain (Bout-Tabaku et al, Pediatric Rheumatology Online Journal 12: 11, 2014).
Specific to the pathology osteoarthritis, both weight gain and loss are related to worsening or improving the conditions leading to pain or pain relief. As little as a 5% gain is associated with the progression of joint degeneration and increased pain. As little as a 5% loss in body mass is associated with less progression in orthopedic joint decay and a reduction in experienced pain (Joseph et al, Arthritis Care and Research 74(4): 860-868, 2022). Further, the magnitude of bodyweight loss affects the magnitude of benefit. In respect to osteoarthritis related joint pain, a weight loss of 10% or more is more beneficial than a 5% loss. One recent study demonstrated that the loss of 20% of body mass in overweight or obese individuals led to about a 25% reduction in pain and a significantly improved quality of life (Messier et al, Arthritis Care and Research 70(11): 1569-1575, 2018).
A collateral benefit of dietary improvement and exercise in older populations is that it can interrupt the association between chronic pain and frailty (Dai, et al, Age and Ageing 53(1): afad256, 2024). Some of this benefit is likely the result of improvements in the obesity : pain relationship but it is also mediated by the bidirectional and destructive sarcopenia : pain relationship. Sarcopenia, the loss of individual muscle cells, is the long term and catastrophic form of muscle atrophy in aging. Atrophy is driven by a sedentary lifestyle and is the loss in size of muscle fibers and, by extension, whole muscle; when we don’t load muscles they lose mass and functional ability. Correlational research has demonstrated an association between sarcopenia and chronic pain. In the elderly ongoing sarcopenia seems to increase chronic pain, and chronic pain inversely appears to increase sarcopenia (Chen, et al. Journal of Pain Research 16: 3569-3581, 2023). Obesity, inactivity, and pain are the perfect storm in the production of a chronically unhealthy and malfunctioning body.
Poverty and pain
We do have to consider a peripheral issue specific to the aged. Poverty is related to increased pain (Glei & Weinstein, PLoS One 16(12): e0261375, 2021). It is also directly associated with a poor diet (Drewnowski et al, American Journal of Clinical Nutrition 79(1): 6-16, 2004) and low to absent leisure time physical activity and exercise (Vancampfort D et al, International Journal of Behavior, Nutrition, and Physical Activity 14(1): 6, 2017). The sheer number of people that are likely affected by the terrible combination of low income, poor nutrition, sedentary life, and the progression of arthritis and pain may be surprising. US Census bureau data indicates there are about 58 million over 60s in the USA. Of that group, more than 17 million (29.3%) are at or below the poverty level. Given their financial straits, it is unlikely that these individuals will be confident enough in their personal finances that they will spend limited income on gym memberships (or home exercise equipment), will make healthier and thus more expensive food purchases, nor will they likely have access to and be able to take advantage of modern anti-obesity drugs (unable to afford).
Pharmaceutical Interventions
Anti-obesity drugs are not new. The first commonly used weight loss drugs were amphetamines, first released in the 1930s, their use in weight loss peaked from the 1950s to 1970s after which safety concerns massively reduced their prescription for such a purpose. There has been a host of pharmaceuticals developed and released into the marketplace in the ensuing years, with a current media frenzy manifesting over glucagon-like peptide-1 (GLP-1) agonist drugs and their ability to drive satiation (not being hungry) as a means to control Type II diabetes and obesity.
| GLP-1 Drug | Brand Name |
|---|---|
| Dulaglutide | Trulicity |
| Exenatide | Byetta, Januvia |
| Liraglutide | Saxenda, Victoza |
| Semaglutide | Ozempic, Wegovy |
| Tirzepatide | Mounjaro |
Weight loss from GLP-1 drugs is well documented, but it, the drug alone, is not the magic weight loss pill portrayed in advertising. A “real world” assessment of the amount of weight lost by obese individuals (average bodyweight 108 kg/238 lb with an average BMI of 37) found that the amount lost depended on the drug, dosage, and duration of the course of therapy but the total amount lost was generally small (White GE et al, Obesity 31(2): 537-544, 2024):
At 8 weeks of administration | 1.19 kg/2.62 lb body weight lost (1.1%)
At 72 weeks of administration | 2.38 kg/5.23 lb body weight lost (2.2%)
These data do not shout “super effective”, as the average amount of weight loss noted at both 8 and 72 weeks can be delivered by a simple restriction diet of some logical type within 2-8 weeks. In a recent meta-analysis of dietary studies, it was determined that the average rate of weight loss per week across interventions was about 1.13 kg (2.49 lb) per week (Finkler E et al, Journal of the Academy of Nutrition and Dietetics 112(1): 75-80, 2013). Note that such data represents the mid-point peak of a standard bell curve distribution. On a simple diet, some people will lose much more than 1.13 kg per week, some may lose virtually none. While the weekly weight loss averages for pharmaceutical treatment with GLP-1 agonists alone are lower than dietary intervention alone with average loss rates between 0.033 kg/week and 0.149 kg per week, a range of better and worse outcomes are normal. In White’s 2024 paper, although the average weight lost was much lower than advertisements suggest, approximately one third of the subjects lost 5.4 kg (11.9 lb) within 72 weeks while on the GLP-1 drug, or approximately 0.075 kg (0.165 lb) per week.
As indicated earlier, a significant number of older individuals are near or below the income level indicative of poverty. As such the cost of GLP-1 agonist therapy is likely cost prohibitive:
Mounjaro = $255.76 per weekly dose
Ozempic = $242.13 per weekly dose
Trulicity = $246.80 per weekly dose
Wegovy = $337.25 per weekly dose
Note: Above are recent manufacturer list prices for the USA, actual costs may vary.
The cost of using the most expensive GLP-1 drug, Wegovy, calculates out to $17,527 per year. Given that the loss of 5% of body weight seems to be the critical low mark of loss for improvement in pain and osteoarthritis status, and given it takes about 72 weeks of drug use alone to elicit a 5% weight loss, the cost of losing about 5.4 kg (11.9 lb) is $24,282. It is absolutely unlikely that an older individual with low to moderate income status could afford to spend this amount on any single drug expense. The average median income of persons 65 years of age and older is approximately $29,740 annually. A $17,527 yearly price tag is not viable in this group, as it represents 58.9% of total annual income. Even non-aged populations may be priced out of this medication given that the annual drug cost is equivalent to 41.5% of the median personal income in the USA (2023), $42,220 for working ages.
Less expensive work arounds
Not being able to afford the latest pharmaceutical should not be a problem. If you watch the GLP-1 agonist commercials on TV and the internet you will note that the small print and fast talk states that the drug is intended to be taken only while on a weight loss diet and when accompanied by some form of regular physical activity, exercise, or sport participation. When all three are combined, the weight loss driven by dietary modification, the weight loss driven by exercise caloric expenditure, and the biochemical effects of the drug produce an additive effect result. In respect to which factor is most powerful in producing weight loss, dietary restriction to between 800 to 1,200 kcal (calories) leads to the most dramatic and timely losses of body mass. However, such a diet is problematic as restricted calories or restricted food choices to such low levels are not maintained easily as a long term lifestyle. Further, they require a great deal of food choice planning in order to get adequate nutrition included in what is eaten and the amount eaten comes in under the caloric limitation. Eight hundred calories can be far less than the calories in many restaurant hamburgers (Wendy’s Baconator comes in at 1010 kcal and a Burger King double Whopper is 942 kcal; an Italian BMT from Subway is 1890 kcal). Eating out is generally not in the cards for individuals on a very low calorie diet … until the individual quits the extremely low calorie diet within three to six months after starting it and regains the weight lost over the ensuing months and years. Also, there are better options than simply slashing calories consumed.
Exercise is slightly more effective than GLP-1 agonists in reducing bodyweight but less so than robust dietary modification. Unlike subtracting calories from the normal diet, simply adding in a mile of walking five days per week expends between 500 and 625 kcal (100 to 125 kcal/mile times 5 days). Adding even such low levels of exercise to normal activity levels can allow less draconian calorie restriction in prescribed diets, giving the individual a better chance at continuity of weight loss and long term maintenance. Combining two or all three methodologies produces a synergistic effect producing slightly larger amounts of weight loss than diet alone, exercise alone, or GLP-1 drug alone.
So, the bottom line here is that pain related to obesity during old age can be reduced or possibly eliminated in a variety of ways, with each method intending to produce the same outcome; to drive enough weight loss to reduce the amount of pain experienced.
If money is tight, diet and exercise can produce 100% of the desired weight loss outcomes, no drugs are required. This is the most fiscally responsible approach, an essential consideration in older individuals on fixed incomes. However, this is the case IF, and ONLY IF, the programs of diet and exercise are designed for weight loss and are adhered to over many months and years. It requires willpower, dedication, and patience to leverage diet and exercise to successfully fight disease, improve fitness functions, and reach vanity goals. If those characteristics are in short supply or absent in an older (or younger) individual, if belonging to a fitness community is not desired or possible, or if the use of a gym membership does not reinforce those traits of sustainability, it is then highly likely that the use of anti-obesity medications, old-school affordable ones or extremely pricey GLP-1 agonists, may be warranted to reduce bodyweight and experienced pain.
| Weight loss method | Average weight lost | Monthly cost for weight lost |
|---|---|---|
| Diet | 1.13 kg/week | $0 beyond food cost for self-directed diet ≈ $100 beyond food cost if nutrition advisor is hired |
| Exercise | 0.52 kg/week | $0 for self-directed walking/running ≈ $25 for pay-for-access gym (e.g., Planet FitnessTM) ≈ $150 for pay-for-results gym (e.g., CrossFitTM) ≈ $250 if personal trainer is hired (1-2 session/week) |
| GLP-1 agonist | 0.149 kg/week | ≈ $1163 |
Interestingly, when prescribed a GLP-1 drug for weight loss, patients are recommended to exercise and begin restrictive diets; generally referred to with a poorly described term “proper nutrition”. Depending on whom is providing advice, proper nutrition could refer to simple caloric restriction, modifying macronutrient composition, or both. If this advice is followed, then the total expenditure on pharmacological treatment of obesity is more than just the drug cost, added costs for gym membership (or home exercise equipment and programming) along with any cost related to dietary changes hikes the price tag.
Another compelling issue to consider is in regards to an extremely troubling side effect of GLP-1 category weight loss drugs, you do not lose fat mass only. A number of research publications have reported that lean body mass, including muscle mass, is reduced, representing anywhere from 15 to 60% of weight lost (reviewed Neeland, et al. Diabetes, Obesity and Metabolism 26(Supplement 4): 16-27, 2024). Any fractional loss of muscle mass moves the patient towards atrophy/sarcopenia induced frailty, and as stated earlier frailty is associated with increased chronic pain. So, it is quite possible that GLP-1 agonist drug induced weight loss may not be the panacea for weight loss and improved quality of life. The patient may weigh less but the side effects may themselves block any weight-loss related reduction in chronic pain … and it is highly probable that physical work capacity will go down as a result of GLP-1 related muscular atrophy.
Start early to stay off drugs
So how much value does an elderly person put on pain relief? Enough to start a program of physical activity, exercise, or sports participation? In general the answer is no, despite over half a century of public service messaging.
The “gold standard” of advice, the Surgeon’s General recommendations, have not worked. The basic and minimalist “just do something, anything that gets you to move for 60 to 150 minutes per week” has largely been ignored by the public. It always will be. The unattained “goals” and recommendations espouse are not those that the general public are affected by, in respect to engaging in anything physical. They are the result of non-directional, non-replicated, and often very small scale experimentation, interpreted through the lens of academia’s publish-or-perish mind-set and for-profit medicine. The results, as you can see below, is a population that is, by majority, absolutely or functionally sedentary.
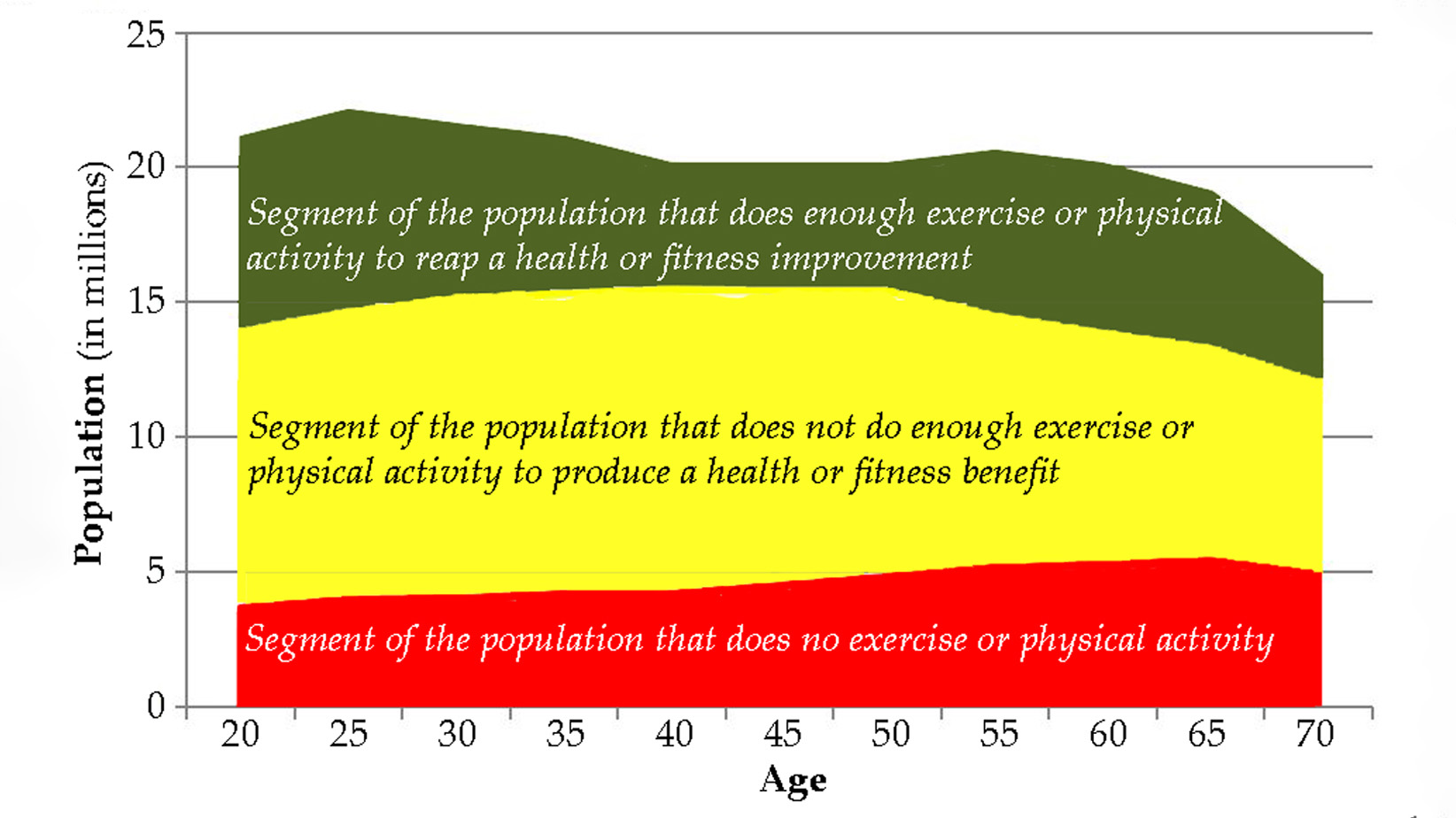
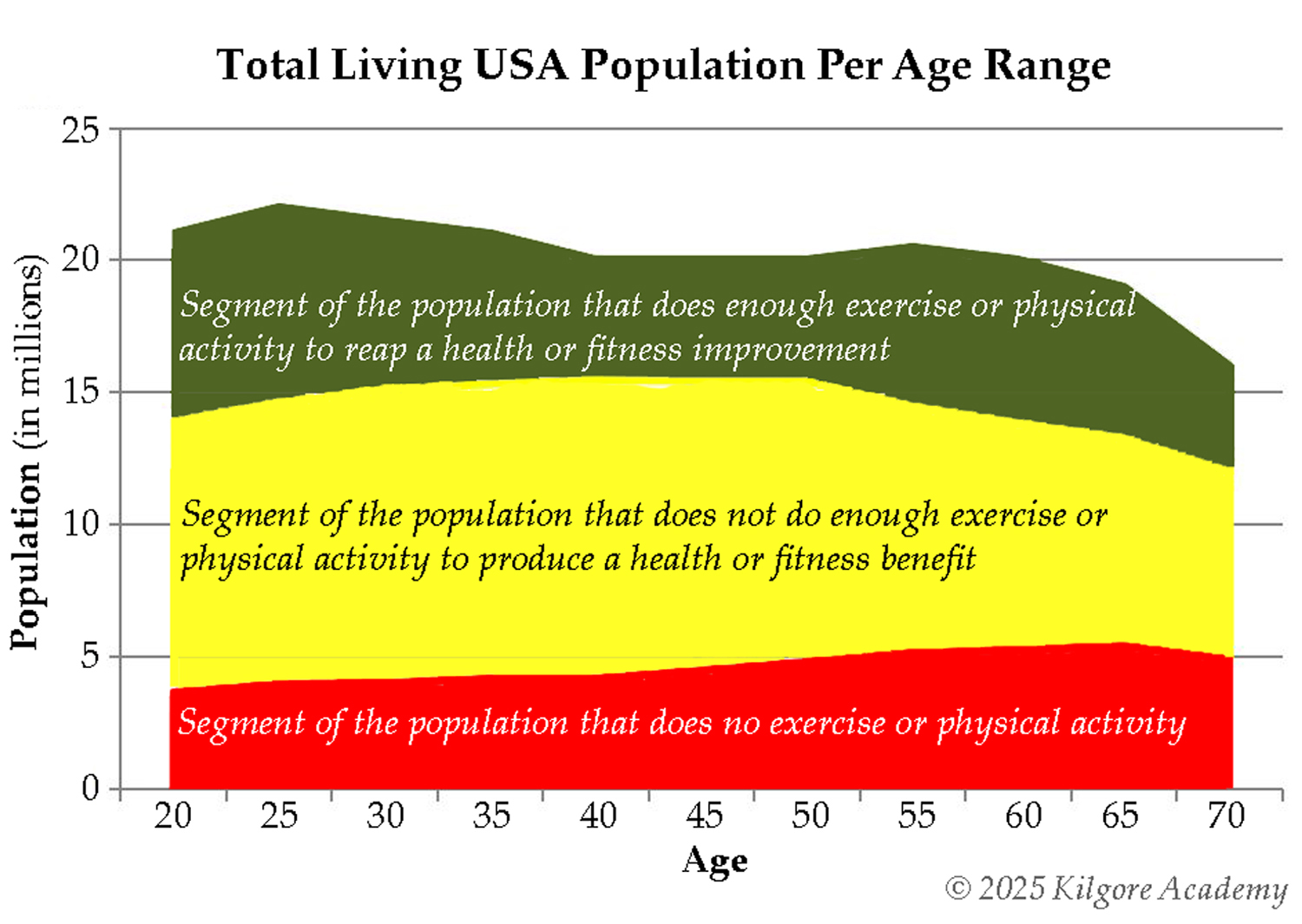
Figure 1. Summative representation of the absolute numbers of how many Americans meet any government or clinical guidelines for engaging in physical activity, exercise, or sport. The number of individuals that are completely sedentary slowly and steadily grows over the lifespan (red area). Those that do some exercise, physical activity, or sport (weekend warrior type) but not enough to produce a tangible health or fitness benefit is the largest segment of the population at any age (yellow area). The segment of the population that does enough to produce fitness or health improvement (green area) diminishes relatively steadily after age 25.
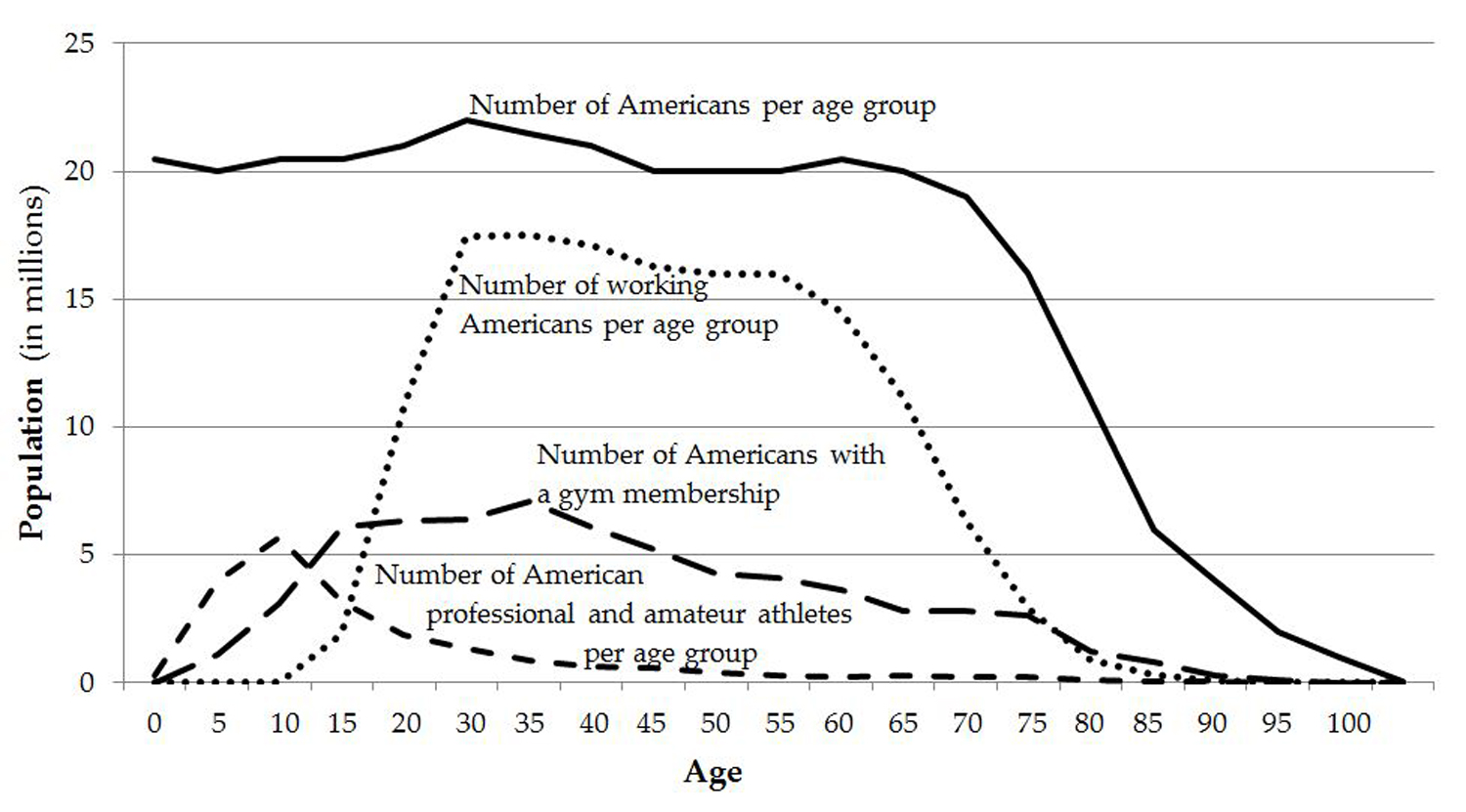
If we look at definitively goal oriented sports participation data we see that professional and amateur sports competition and training does not attract a majority of Americans. By the late teens, participation in organized sport and competition begins to wane dramatically, dropping from nearly 6 million teens to a little over 1 million adult sports participants by their early 30s, to about a half million sportspersons in their early 40s, and to about a quarter million in their early 50s. This slow decay in engagement continues until the late 70s where participation rates decline to next to zero.
Figure 2. Amateur and professional sports appear to cater to younger populations (short dashed line). Professional athletes are currently inconsequential as there are only about 35,000 full and part-time professional athletes in the USA and approximately 55% of them are aged between 20 and 34. Gym memberships (long dashed line) replace sports participation as individuals enter the work space (dotted line) and then membership numbers begin to wane after age 35.
We often think that people who go to the gym have goals that more effectively push them towards longer term fitness training. Starting in the late teens, coincident with entry into the working ages, there is a drift away from sports participation towards commercial gym membership. This is most likely a function of employment time demands draining away adequate time to train for competition. Regardless of source population, athlete or non-athlete, in the late teens about 5 or so millions of that age group are members of a gym. That number continues to slowly rise to over 7 million with gym memberships in the early 30s. That number drops to 5 million again in the mid-40s. By retirement age, membership numbers in the age group are less than 3 million and by the late seventies there are less than 1 million memberships held and within another decade there are virtually zero. While this data is fairly bleak, it can and is likely worse. Only a small fraction of the total population has, is, and will participate in physical activity, exercise, or sport to the level of volume and intensity required to both produce fitness and reduce pain. Note that less than half of gym members exercise two or more times per week (meaning that more than half train one time or less per week). Further, that data is for those that actually go to the gym. If, as some fitness industry estimations suggest, nearly 67% of gym membership holders do not actually go to the gym and 50% of all new memberships are cancelled within 6 months, the data is damning for participation numbers.
It is obvious that the Surgeon’s General position and recommendations, while nobly intended, are inadequate in application. There is a need for better research and a massive change in approach to improving public engagement in any type of movement.
For most things in life, establishing a good foundation creates longer term success. In the context of lifelong engagement in exercise, a recent study provides us with an inkling of how we might proceed to create a more active population throughout the lifespan (Dohle & Wansink, BMC Public Health 13: 1100, 2013). In that study a correlation was demonstrated where children and teenagers who competed in youth sports were far more likely to be exercisers in their 70s than youth who did not participate in sports. This is an interesting relationship that needs experimental exploration and replication.
So, it appears, on the face of this research, that getting young children to play sports may be a key factor in setting the stage for a lifetime of healthy sport, exercise, and physical activity; a lifetime with lesser pain at every stage. So let’s get more children involved in more physical education and more sports to create better later in life outcomes.
This poses a large problem, as primary and secondary education institutions and government oversight bodies have a long history of reducing or eliminating physical education requirements, staff, and funding. Sports participation in schools has seen similar reductions, on top of already having a limited number of sports and spots on those teams. Sometimes the discontinuation of school sports is framed in the idea that sport is not contributory to education. Sometimes the decisions are based solely on financial issues, where removal of sports decreases school operational costs or it significantly reduces insurance costs (less legal exposure to liability and thus lower premiums).
If we are serious about leveraging early life sport participation into lifelong health and fitness, we must rethink school-age sports and physical education and remove the negative cultural and social stigmas of being a “jock”. Moreover, investment in our children is needed; this means the hiring of competent physical educators and coaches is required to steer away from one educator or coach working with 50 to 100 students at a time with limited to absent resources. Kids hate PE because it can’t be individualized or optimized to provide a useful and enjoyable experience within current constraints (there are very rare but laudable exceptions out there). Also, when the majority of parents and administrators see no down side to reducing the presence of PE and sport in schools, then we cannot expect students to embrace either as important elements of a healthy and happy life, in the short term or long.
So, for the present cohort of older individuals with pain we can only urge them, persuade them, to start exercising and eating better (not just eating less) as a means to reduce experienced pain as fitness increases and bodyweight goes down. This is a difficult task that will have limited success BUT any success, or successes, is progress and will be life changing. However, to create a better future for those who are young now, the entire system needs revision to create more and better opportunities for our youth, and even our young adults, to stay active regardless of any stage of life challenge facing them. Act youthfully to benefit agedly.
Lon Kilgore earned a Ph.D. from the Department of Anatomy and Physiology at Kansas State University’s College of Veterinary Medicine. He has competed in weightlifting to the national and international level since 1972 and coached his first athletes from a garage gym to national-championship event medals in 1974. He has also competed in powerlifting and currently holds several continental and world records, won his division in the first CrossFit Total event, was a decent high school wrestler, caught a number of crabs during his short collegiate rowing stint, was and still is a hack at golf, and was a regional fish cutting champion and competitor at nationals. He has worked in the trenches – as a qualified national-level coach or scientific consultant – with athletes from rank novices to the Olympic elite, and as a consultant to fitness businesses. He was co-developer of the Basic Barbell Training and Exercise Science specialty seminars for CrossFit (mid-2000s) and was an all-level certifying instructor for USA Weightlifting for more than a decade. He is a decorated military veteran (sergeant, U.S. Army). His anatomical illustration, authorship, and co-authorship efforts include several bestselling books and works in numerous research journals. His fitness standards for weightlifting and calisthenics have been included in textbooks and multitudinous websites. After leaving a 20-year plus professorial career in higher academia, his teachings can be found in vocational-education courses offered through the Kilgore Academy, and in articles like these.
Support the Broken Science Initiative.
Subscribe today →
2 Comments
Leave A Comment
You must be logged in to post a comment.
recent posts
And more evidence that victory isn’t defined by survival or quality of life
The brain is built on fat—so why are we afraid to eat it?
Q&A session with MetFix Head of Education Pete Shaw and Academy staff Karl Steadman

Very impressive resume Dr. Kilgore. Loved the informative article!!
I agree very informative article.