It’s not breaking news that medicine in the US today needs a makeover. We’ve become a nation of far too many overweight, out-of-shape, and chronically ill citizens, both young and old; a trajectory that is non-sustainable. One reason for this sad state of affairs is the near-complete financial capture of everything that touches health care: the media, academia, research, medical journals, and the governmental regulatory agencies, all of which has led to a misguided groupthink that the solution to all diseases lies in finding another pill, injection, or vaccine.
Americans already spend twice (or more) as much per capita on health care as Europeans and Canadians do, and yet have poorer average health and longevity to show for it.
A MedScape Scenario
The issue was exemplified by a MedScape quiz sent out recently concerning the proper next steps to address the persistently elevated blood pressure of a patient named Thelma. Her history was described in the introduction thus:
“Thelma has had check-ups every 1 or 2 months for 5 months now, and her hypertension continues to be an issue. Her workup for secondary hypertension was negative. Her daily regimen now includes losartan (100 mg), hydrochlorothiazide (25 mg), and amlodipine (10 mg). However, her blood pressure remains elevated. Her office blood pressure is 144/90 mmHg, and she completed an ambulatory blood pressure monitor test which showed an average blood pressure of 138/84 mmHg, with less than 10% dipping at nighttime. Her pulse rate ranges from 68 to 83 beats per minute.
She remains asymptomatic and adherent to her medications. She has tried to eat a more plant-based diet and has lost 1 kg in the past 5 months. An estimated glomerular filtration rate completed 2 weeks ago was 48 mL/min/1.73 m² (reduction of four units from 5 months ago), and her potassium level is now 4.2 mEq/L.”
The slight drop in her eGFR (an estimated measure of kidney filtering capacity based on the person’s creatinine measurement) is likely not all that significant. The eGFR can vary a fair bit due to lab imprecision, the person’s hydration status, diet, other concurrent illnesses that may be present, and day‑to‑day creatinine fluctuation, even when true kidney function is stable.
In a nutshell, this lady’s story is that she has been worked up for causes of secondary hypertension with none found, put on three prescription medications to control her pressure, told to ‘eat a more plant-based diet’ which she’s tried to do, and been followed monthly for 5 months. And despite this standard of care treatment she’s lost but 1 kg and her pressure is still not where her physician would like to see it, even though it is not outrageously higher than the 130/80 the ACC and AHA now recommend as ‘controlled’ hypertension.
So the dilemma is what to do next. And the first question of the MedScape quiz offers the clinician four choices as to what that should be. Choices 1, 2, and 3 are each the addition of a fourth pill to control her pressure—add atenolol 25 mg a day, add hydralazine 25 mg three times a day, or add spironolactone 25 mg a day. And the fourth choice is outrageous – refer her for evaluation for renal denervation, basically a procedure to destroy the sympathetic nerve input and output from her kidneys. Pretty extreme for a pressure mildly above what you’re aiming for and what looks to be stable kidney function.
This quiz exemplifies the kind of not-so-subtle brainwashing that passes itself off as continuing medical education. And it’s unconscionable. Why?
To begin with, she’s asymptomatic, they say and has ‘remained so’ which suggests that she was asymptomatic from the jump, and perhaps her high pressure reading was discovered incidentally. But medical management has abandoned the notion of looking at and treating the whole living person; too often it’s become an exercise in number chasing—whatever it takes, however many pills or shots need to be piled on to get a cholesterol under 200 mg/dL, get an LDL under 70 mg/dL, get a blood pressure under 130/80 mmHg.
And it’s illuminating to point out that not so very long ago a blood pressure reading of 140/90 was considered normal, and it still is considered normal in Europe and Japan where general health and longevity is better than ours. Now in the US, however, it’s been codified as a cause for three (or four) medications a day and a possible renal denervation procedure. How did that happen? Pharma capture of the narrative is how.
What could we do to help Thelma?
The introduction doesn’t tell us anything about Thelma’s physical state or other lab values. Is she overweight? (probably) Sedentary? (probably) Is her insulin elevated? (probably) Are her glucose or triglycerides high? (probably) Does she have a high waist circumference, reflective of excess storage of visceral fat and fatty liver? (probably). And if so, all of that points to underlying Metabolic Syndrome (MetS). Did they look at these things in that light? We don’t know, but they should have.
When secondary causes of hypertension have been eliminated, as they tell us they have been with Thelma, the likeliest root cause is MetS – i.e., insulin resistance – and its effects that cause the kidneys to hold onto sodium and excess fluid, among many other physiologic changes that may result in blood pressure elevation as a manifestation of the metabolic dysfunction.
And fortunately there’s a simple fix for that, but it doesn’t come in a gelatin capsule, tablet, or syringe, so there’s no corporate profit in it. It comes in a ‘Box’. It’s a whole food, protein-and-fat-rich, low-carb, ketogenic diet plus functional movement (aka MetFix methodology). Instruct Thelma to eat meat, fish, poultry, eggs, dairy, nuts, seeds, fresh vegetables, little fruit, little starch, and no sugar for a month. Have her keep a careful journal of what she’s eating every meal, because doing so increases the chance of success in implementing a lifestyle change. Get her off the couch and into the Box, and watch what happens. This approach will most assuredly reap more than a 1 kg weight loss in 5 months and countless other benefits to her health and longevity.
But changing Thelma’s diet and adding resistance training and functional exercise was nowhere to be found on that approved list of correct next steps, even though a low-carb/ketogenic diet has been shown in repeated clinical trials to improve or resolve most of the symptoms of MetS. It predictably offers quick reduction of elevated triglycerides, blood sugar, and insulin. HDL typically rises (and not much else does that but exercise). There will be weight loss and girth loss. If present, GERD improves. And in many cases (though not all, but about 80 to 85% of them) it markedly reduces blood pressure as well.
As a colleague once said to a group of physicians not yet acquainted with the power of the right nutritional structure: nothing in your experience will prepare you for how quickly this diet will work.
In fact, if her hypertension responds to the diet, it could drop her pressure so quickly that she will need to be weaned off her pills or risk falling on her face when she stands up! In our clinical practice we removed diuretics immediately upon commencing the diet and tapered other antihypertensives that might cause rebound in the pressure if removed abruptly. Our goal was always to get rid of pills, not to add another.
Sadly, this scenario isn’t rare. The country is filled with Thelmas. And all of them deserve a chance to get off the add-a-pill carousel and reclaim their health and fitness with good nutrition and proper exercise. And that’s where MetFix comes in. It’s not always easy, but it’s simple. And amazingly effective.
Physician, author, blogger, and lecturer on the art and science of low-carbohydrate nutrition, using food as a remedy for the diseases of modern civilization: obesity, diabetes, heart disease, and the myriad disorders of the insulin resistance/metabolic syndrome complex.
Support the Broken Science Initiative.
Subscribe today →
recent posts
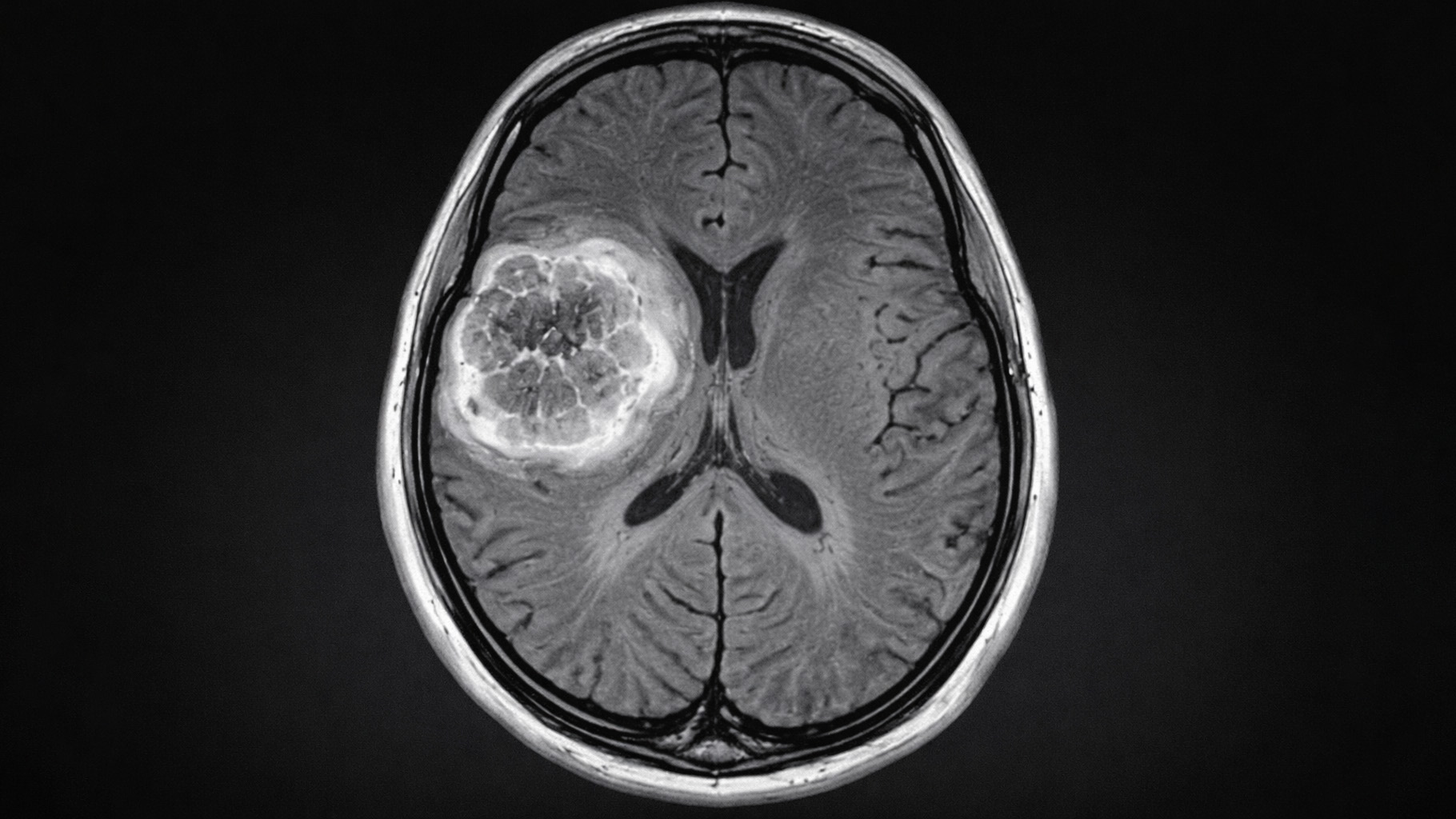
And more evidence that victory isn’t defined by survival or quality of life
The brain is built on fat—so why are we afraid to eat it?
Q&A session with MetFix Head of Education Pete Shaw and Academy staff Karl Steadman